The Vital Human Organ That Can Miraculously Regenerate
The liver is one of the most important organs in the body, yet many people are unaware of its true function. Simply put, the liver serves as a filter for the blood. In conjunction with the kidneys, the liver clears the blood of harmful compounds and releases them in bile into the small intestine. From there, the small intestine expels that bile as waste. That being said, the liver serves numerous other functions as well, including the production of certain proteins, the regulation of amino acids, and the storage of hemoglobin.
Thus, virtually anything you ingest that enters the bloodstream is processed by the liver. Yet, while healthy organic compounds are easily processed, many of the compounds in the modern diet can be taxing enough on the liver to cause damage. These include alcohol, trans fats, excessive vitamin supplements, sugar, and even acetaminophen (also known as Tylenol or paracetamol). Essentially, any compounds that the liver struggles to process can cause the organ to inflame. That swelling can cause tissue damage. In most organs, tissue damage alerts the immune system to take action. The liver, however, has its own unique regenerative response that can repair its own tissues.
Skin cells regenerate fast and on a fixed schedule, and even kidneys can heal themselves from minor damage. However, the liver is the only organ in the human body that can regenerate its tissues in response to extensive damage. The liver's regenerative abilities are so strong that even large sections can grow back if given the opportunity. Some studies have suggested that up to 90% of the liver can regenerate after being removed. While scientists have been aware of this special, "miraculous" ability for a long time, the cellular mechanics behind the phenomenon have only recently been unveiled.
The newly discovered mechanics of liver regeneration
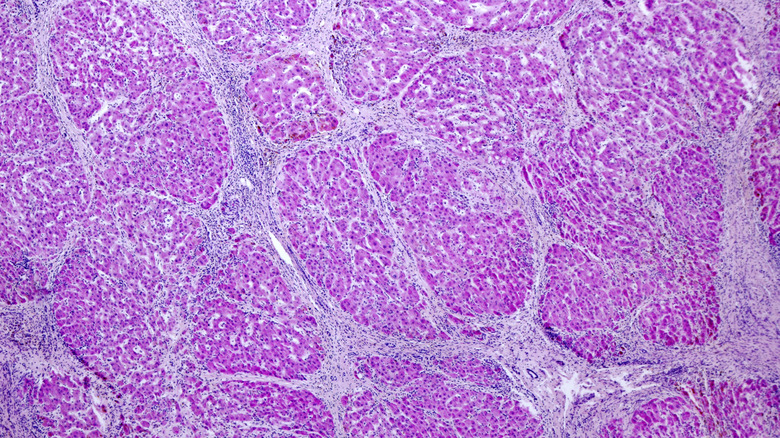
It makes sense that the liver should possess the ability to regenerate, considering its job in filtering harmful toxins. About 80% of the liver is composed of cells called hepatocytes, which are the main line of defense against toxic compounds. As toxins in the blood pass through the liver, liver cells can be destroyed. But their sacrifice isn't in vain. The damaged hepatocytes release protein signals to surrounding cells to carry away the waste in bile, which also triggers an inflammatory response to fill in the gaps. Within seconds of exposure to toxins, liver cells begin the tasks of replication and waste disposal.
While this regeneration process had been observed for a long time, there has been an ongoing debate about whether stem cells or hepatocyte cells are responsible for the creation of new healthy liver cells. Published in Science in 2021, a breakthrough study demonstrated that hepatocytes performed the majority of the work in regenerating damaged liver cells. The process was observed to occur in "zone 2" of the liver, where liver cells are located between the enzyme-producing zone 1 and the waste-disposing zone 3. Essentially, the liver's mid-section takes on the brunt of the organ's maintenance, ensuring that toxin-damaged cells are replaced with healthy new ones before the immune system's scarring response is triggered.
The study confirmed that the liver is indeed self-healing, using its own cells for maintenance. However, it also demonstrated the limits of liver regeneration. Because zone 2 liver cells are shielded from direct exposure to toxins by zones 1 and 3, the cell-signaling pathways that alert the zone 2 cells to jump into action are vulnerable to permanent damage.
The limits of liver regeneration
Many of the most common habits that increase the risk of an early death are related to damage to the liver. These include extreme diet trends, alcohol, drugs, and even the excessive consumption of supplements. But if the liver can regenerate, how could such habits cause long-term problems?
While studies have shown that hepatocyte cells are capable of unlimited regeneration, the process is extremely slow. When damage is chronic, the hepatocyte cells don't have enough time to duplicate and replace damaged cells. In such cases, liver cells will inflame to temporarily occupy the missing space. While such inflammation temporarily restores the volume of the liver, it doesn't restore the number of chemical pathways for signaling. When inflammation is prolonged, the immune system kicks in and replaces the inflamed tissue with enlarged scar tissue. The result is fibrosis and cirrhosis, which are irreversible side-effects of acute liver damage.
When scarring forms before the liver can regenerate, the chemical pathways used for signaling are compromised. This results in a higher risk of liver neoplasia, or abnormal cell growth, which can ultimately lead to liver cancer. Thus, while the liver can "miraculously" regenerate, there's a speed limit. Chronic exposure to toxins may be too fast for liver cells to replicate before the immune system begins replacing damaged tissues with scar tissue. At the end of the day, the liver is self-healing, but it's not invulnerable.